Zenaida Chapman with the CRSHE
Uterine fibroids are a reproductive health issue that remains largely unknown, underdiagnosed, and under-researched. Although about 80% of women develop uterine fibroids, their underlying causes and impact are still not well understood.
This blog post will break down what uterine fibroids are, who is most affected, and the impact they can have on overall health and quality of life while also exploring preventive steps and treatments that can help.
What are Uterine Fibroids?
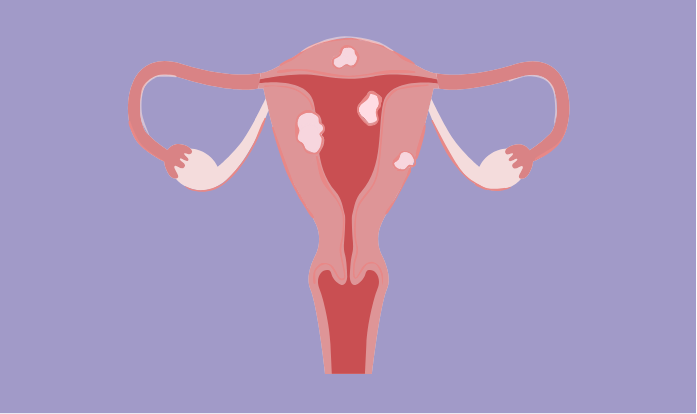
Uterine fibroids are growths made of fibrous connective tissue and smooth muscle cells. They vary in size from as small as a seed to as large as a melon and can grow individually or in clusters. They may appear in the uterus, within the uterine wall, or on the surface of the uterine wall. The size and structure of fibroids make them difficult to detect, which is why so many of them go unnoticed. Up to 80% of women will develop fibroids sometime during their childbearing years, however only about a third of these fibroids are large enough to be detected during an exam, which means they often go undiagnosed and therefore untreated.
How are women affected by uterine fibroids?
Symptoms of uterine fibroids can vary widely. Some women experience severe symptoms that significantly impact their quality of life, while others may have no symptoms at all. The severity and type of symptoms largely depend on the size, location, and number of fibroids. Common symptoms include:
- Heavy menstrual bleeding and cramps: Fibroids can cause painful and prolonged periods which can lead to anemia or increased fatigue.
- Pelvic pain: Fibroids can cause dull or sharp pelvic pain (often linked to menstrual cycle).
- Urinary issues and constipation: Fibroids can press on the bladder area or bowels, causing incontinence, constipation, or general pelvic pressure/discomfort.
- Impact on fertility: Fibroids that press on the endometrium, the inner lining of the uterus, could interfere with the implantation of an embryo, potentially decreasing the chance of getting pregnant.
- Sexual impact: Fibroids can cause pain during sex, leading to reduced sexual satisfaction and emotional stress associated with intimacy.
What are they caused by?
Although the exact cause for fibroids remains unclear, it is believed that a combination of genetic, hormonal, and environmental factors lead to their development. It’s established that they are influenced by hormones (progesterone and estrogen), their growth being correlated with hormonal changes. For example, fibroids tend to grow during pregnancy (when estrogen levels are high) and regress after menopause (when estrogen levels drop), which is an important link for exploring possible effective treatments.
What are the risk factors?
Certain factors increase the likelihood of developing uterine fibroids, and understanding these risks is crucial to better prevention and treatment. While the exact causes remain unclear, the following factors have been identified as contributing to higher rates of uterine fibroid development:
- Ethnicity: African American women are at the highest risk for developing fibroids due to genetic and hormonal factors.
- Family history: Having close relatives with fibroids increases the risk with genetic predisposition playing a significant role.
- Age: Prolonged exposure to estrogen due to early menstruation or late menopause increases the chances of developing fibroids.
- Hormonal imbalances: Imbalances in estrogen and progesterone contribute to fibroid development, with fibroids growing in response to elevated estrogen.
- Obesity: Women who are overweight or obese are at higher risk of developing fibroids.
- Diet: A diet high in red meat, processed foods, and low in vegetables may increase the risk of fibroids.
- Vitamin levels: A deficiency in Vitamin D and excessive levels of Vitamin E are linked to fibroids.
What are the preventative measures and potential treatments?
There’s no “one size fits all” approach to treating uterine fibroids. Options range from lifestyle changes, to pain management, to hormonal treatment, to surgery, depending on each woman’s unique symptoms, risk factors, and fertility goals. Uterine fibroids are the leading cause of hysterectomy in the U.S., but the question remains: How can we increase options for women who suffer from uterine fibroids and want to preserve their fertility?
Hysterectomy, removal of the uterus, remains the most definitive treatment, however, new treatments and advancements in reproductive technology may allow for fibroid symptoms to be managed without affecting fertility. As the medical field advances, new treatments to shrink fibroids and manage symptoms are being explored to offer more choices for women.
Preventative Measures:
- Diet: A balanced diet full of fruits and green vegetables with less red meat and processed foods might lower the risk of fibroids.
- Exercise: Regular physical activity may help maintain a healthy weight, helping minimize fibroids risk.
- Hormonal control: Hormonal birth control methods can help regulate estrogen levels and reduce the development of fibroids.
Medication-Based Treatments
- Pain relief: Over-the-counter anti-inflammatory drugs like ibuprofen can help with cramps and heavy bleeding, but don’t shrink fibroids.
- Hormonal treatments: Options like birth control pills, hormonal IUDs, and progesterone-based treatments can regulate bleeding.
- GnRH agonists/antagonists: More recently developed medications that mimic or block GnRH decrease estrogen levels which shrinks fibroids (these are usually short-term solutions before surgery due to side effects).
Minimally Invasive Procedures
- Myomectomy: This surgery removes fibroids while keeping the uterus intact. It can be done through a few methods including open surgery or hysteroscopy (through the vagina) depending on fibroid size and location.
- Uterine artery embolization (UAE): A procedure that cuts off blood flow to fibroids, causing them to shrink over time.
- Radiofrequency ablation: A newer technique that uses heat to shrink fibroids without harming surrounding uterine tissue.
The best treatment depends on fibroid size, symptoms, and personal fertility goals of each individual. While some women can manage fibroids with medication or lifestyle changes, others may need surgical options. The key is having open discussions with healthcare providers and increasing education on available options to find the right path forward. Increasing education and awareness about uterine fibroids, as well as supporting the development of possible new treatments, will be essential in helping women make educated health decisions.
Final Thoughts
While uterine fibroids remain a common concern for women, ongoing advancements in treatment methods offer more options for managing symptoms. As we continue to raise awareness for under-explored women’s reproductive health topics, it is crucial to remember that each experience is unique. Every woman’s journey with fibroids can look different based on factors like age, ethnicity, and fertility goals. Even when it comes to treatment, what works for one woman may not work for another. Some women may experience severe symptoms, while another may experience no symptoms at all. It is crucial to approach each case individually, ensuring women have access to the information and resources they need to make informed choices about their health.
Looking ahead: Moving forward, the conversation around reproductive health expands beyond uterine fibroids to explore how the reproductive system is connected to diseases that disproportionately affect women, such as autoimmune disorders. The link between reproductive health and conditions like lupus and rheumatoid arthritis raises important questions about how these diseases intersect with women’s reproductive health. Stay tuned as we dive deeper into the connections between autoimmune disorders and the female reproductive system, exploring their shared risk factors, symptoms, and potential treatments.
Citations and Further Reading
FDA Approves New Treatment Oriahnn for Heavy Menstrual Bleeding Associated with Uterine Fibroids